Missouri is one of eight states that will receive money from a settlement reached Monday with a California company, according to the Missouri Attorney General's Office.
Attorneys general from Missouri, California, Illinois, Louisiana, New York, Texas and Virginia came to the agreement with web-based electronic health records company Practice Fusion Inc. Practice Fusion accepted payments from specific drug manufacturers in exchange for promoting some of the same manufacturers' drugs to physicians using Practice Fusion software.
The promotions (pop-up notifications) suggested to physicians that particular drugs be contemplated as they considered patients' histories, according to a news release from Missouri Attorney General Eric Schmitt's office. Payments that Practice Fusion accepted constituted kickbacks, violating federal law.
"Promoting specific drugs through push notifications in exchange for payments is a violation of multiple state and federal statutes and eliminates the level playing field for the drug manufacturers that did not pay to have their products promoted," Schmitt said in the news release. "The Medicaid Fraud Control United of the Attorney General's Office works hard every single day to root out fraud and recover taxpayer money, and this settlement is yet another product of their dedication."
The violations happened from November 2013 through August 2017.
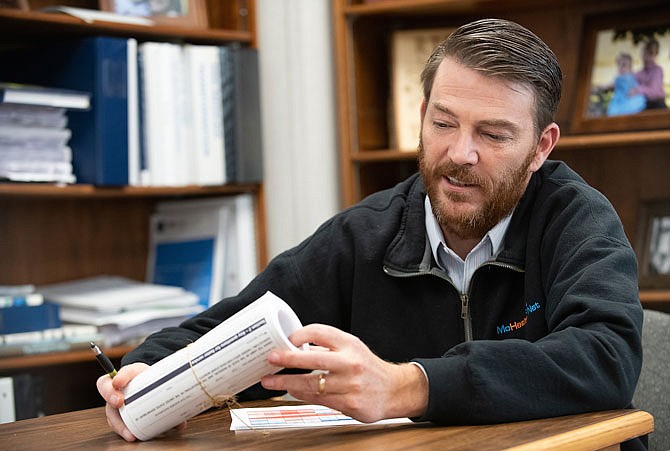
Practice has agreed to pay $5.2 million to state Medicaid programs. Missouri's program, Mo HealthNet, is to receive about $1 million from the settlement. The amount represents about one-ten-thousandth of the state programs annual budget, which is about $10 billion.
The civil settlement resolves allegations the company received improper pay from drug manufacturers based on increased sales from electronic "alerts." Practice Fusion chose guidelines for the alerts, set criteria that determined when providers received them and oftentimes drafted the actual language used in the alerts.
The alerts did not always reflect accepted medical standards, according to the release. And, although they appeared to provide unbiased medical information, the alerts were designed to encourage providers to prescribe a specific drug or class of drugs in some instances, the news release states. Practice Fusion's actions served as an inducement to promote the same companies' drugs through alerts in violation of the Anti-Kickback Statute.
"This behavior," the release states, "resulted in false claims or information being submitted or presented to state Medicaid programs for reimbursement."